
Every day this month I’ve read a news story that tells me the NHS is in crisis - ambulances are lining up outside hospitals, beds are full and there’s less of them than in previous years, there’s nowhere to discharge the individuals in those beds to and there are significant issues with both recruitment and retention of qualified staff to care for those who need it. Increasing demand on services from an ageing population and a net reduction in health and social care spending is causing a perfect storm wherein those individuals who are most in need are unable to access services where they need them, when they need them. If only we knew this was coming then we could have done something about it, right?!
In a recent blog, Chris Ham, the Chief Executive of the King’s Fund – who did predict this scenario a number of years ago - proposed 3 key priorities for tackling these challenges: 1) committing to a long-term plan that provides funding and staffing, 2) improving productivity and extracting as much value out of available spending as possible and 3) reforming the NHS and integrating population health and care to provide greater emphasis on prevention.
In short, priorities 1 and 3 involve taking a long-term perspective that will be unlikely to significantly reduce demand in the short-term. Priority 1 requires finding more money to tackle current and increasing demand. However, with politicians celebrating the money they have made available to help the NHS with pressures this winter - despite providing less than half of what was needed after the crisis this winter had already begun (hardly a proactive long-term strategy) – this priority will be heavily influenced by the political landscape and will take time to have an impact if and when funding changes. Priority 3 involves a focus on prevention that will undoubtedly have an impact in the long-term, but will also see minimal short-term changes in demand. This leaves us with priority 2 - so how do we improve productivity and extract as much value out of what’s available as possible?
In order to deliver major performance improvement, high performing organisations will often consider all of the marginal gains that they may make that will aggregate to a significant improvement – rather than trying to find that one thing that provides significant improvement alone. This approach is known as marginal gains theory, which was brought to public consciousness by Sir David Brailsford – Performance Director of Team Sky and previously of British Olympic Cycling – when taking an ailing cycling team to major Olympic medal hauls (winning 70% of the gold medals on offer in 2012!) and providing Britain with our first Tour de France winner. By optimising everything from nutrition to the ergonomics of the bicycle seat, Brailsford and his team left no stone unturned. If long-term funding and a focus on prevention are the big things that will reduce demand in the long-term, then to reduce demand in the short-term we must ask what marginal gains can be made that - when clumped together - will be able to tackle some of the challenges in demand faced by the NHS and in particular emergency departments.
Our first marginal gains must start by reducing inappropriate attendance at emergency departments. The behavioural insights team at ICE have worked with local authorities, CCGs and NHS organisations to explore the behavioural challenges that lead to inappropriate attendances at emergency departments and to create behavioural solutions to solve them. In many places, we have identified that up to 1 in 3 (>30%) attendances at emergency departments may be deemed inappropriate, with self-care or a visit to another service being a more appropriate behaviour. Imagine the difference having even a 10% reduction in inappropriate visits could make! The insight our team have conducted with citizens has clearly demonstrated that citizens are presented with too much information and too much choice when they need to decide where to go for treatment/support. When faced with a lot of choices, we are unable to fully understand all of the available options and when we have incomplete information, new choices or novel behaviours feel too risky, so we will just do what we’ve always done. This is known as an ambiguity effect and will often lead to a status quo bias wherein we default to our habitual behaviours. For example, most citizens would be unable to tell you what they can visit a minor injury unit for or even when they are open, but they know that if they go to an emergency department at any time during the day or night, they will be seen by an expert within 4 hours (the target the NHS has set itself). When we ask citizens to make this service vs. service decision, the emergency department will always win.
To change this behaviour, we need to change the decision making process. We need to move citizens away from a service vs. service decision, and we need to support the individual to make a condition/symptom based decision. National campaigns such as “Choose Well” do not work because they continue to make citizens choose between services. They ask citizens who believe they are choosing well to choose well and do not provide information or communications that supports them to change this decision - the message frames typically just ask them to stop and think and take responsibility.
ICE have developed an award winning digital solution called ASAP that uses choice architecture to support citizens to make a condition-based decision by utilising behavioural nudges. Within ASAP, a citizen’s choice to search by service is not removed, but a search by condition icon is placed above the search by service icon, making it the default choice and nudging users to search by condition first. ASAP usage data demonstrates the effectiveness of this nudge, with users 3 times more likely to search by condition than by service. For each condition, users are given information regarding the condition (including how to self-care for certain conditions) and are then presented with a list of local services to choose from. The presentation of services is ordered based on which service we want users to use, and an emergency department is not included in the list for conditions that we do not want users to present with at an emergency department.
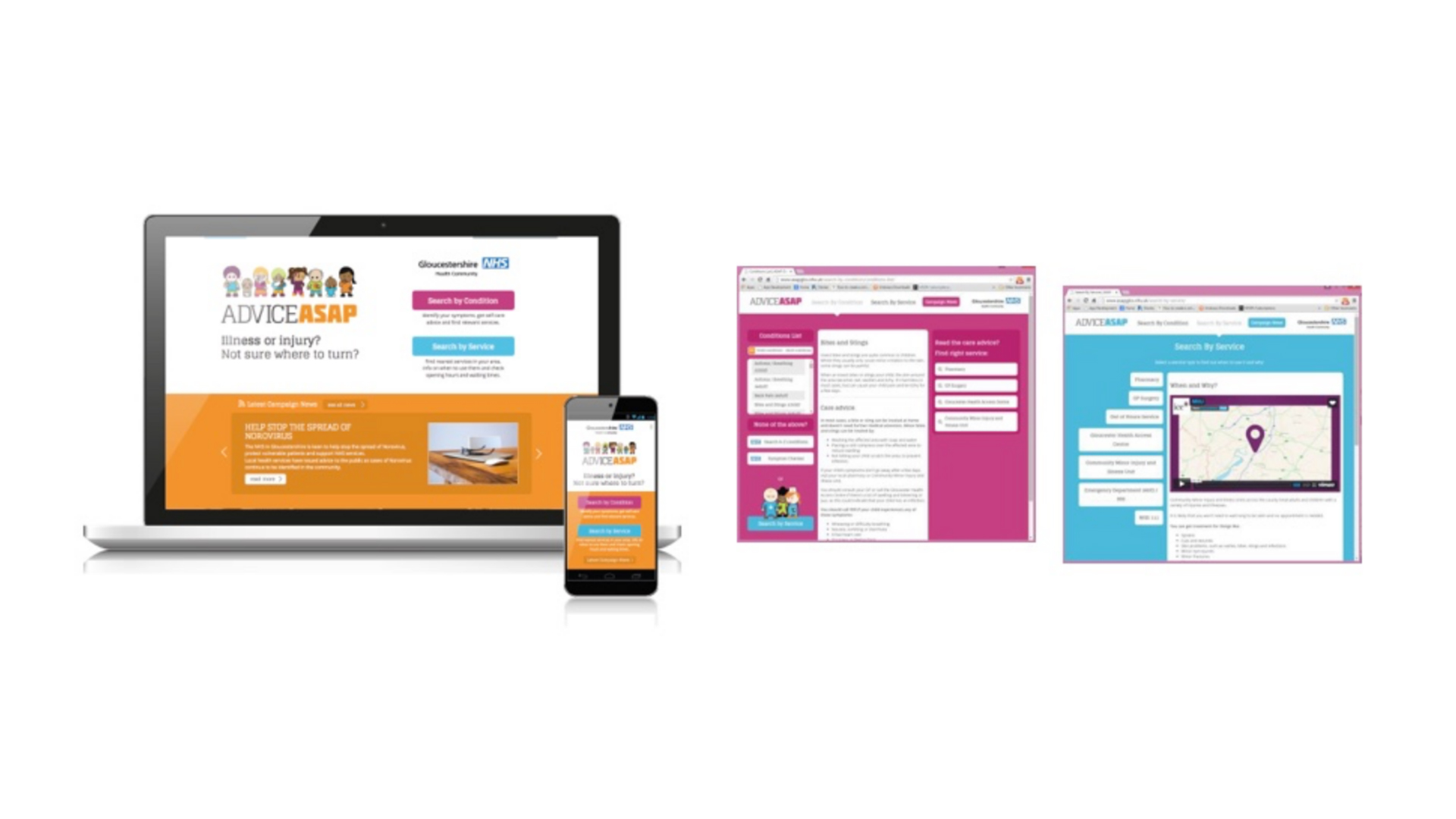
ASAP was developed and implemented in Gloucester. In the 12 months that followed the launch of ASAP, emergency department attendances at Gloucestershire Hospitals NHS Foundation Trust reduced by 7.2% for the target audience of ASAP (0-50 year olds), a result that may be considered even more impressive based on the fact that the year prior to launch had seen an 11% increase for this cohort. Further, attendance at minor incident units – the service G-CGG wanted demand moved to - increased by 7%, suggesting that demand had been successfully shifted across the system.

Whilst digital solutions can provide marginal gains that actually result in big impacts, the ASAP digital solution itself was in fact only one factor in its success. An effective communications and engagement strategy was developed that utilised supportive message frames and visuals that ensured citizens accessed ASAP independently. We also worked closely with leaders and stakeholders to align services and improve signposting, with digital banners shared across websites. The communications and engagement activities also raised awareness of available services and ensured the workforce was changing its conversation with citizens. These are key factors in creating an ecosystem wherein the system is aligned, connecting and making it easier for citizens to navigate it. It is this ecosystem of leadership, culture, communications, engagement and behavioural solutions that can provide multiple marginal gains that provide a big impact.
During 2018, the NHS is expected to launch NHS 111 online. NHS 111 online is being developed by NHS Digital within programme 5 of their urgent and emergency care strategy to transform health and care through technology. To talk to us about how you can use behavioural insights to reduce demand in emergency departments and to prepare for the implementation of NHS 111 online, please contact the ICE team on 0151 647 4700